By Johanna Chelcun, MHS, PA-C and Karen Chelcun Schreiber

For those of us considering undergoing a prophylactic Total Gastrectomy (TG), here are some questions you should consider asking your potential surgeon. It won’t be easy to fit all of these issues into a brief consultation, so make sure to schedule enough time to discuss your concerns – remember, this is a life-altering decision!
We’d all like to have a surgeon who is an expert on our disease. This may be difficult, though, when the disease is as rare as HDGC. Depending on the size and location of the medical center, you may be working with a surgeon who is experienced in performing total prophylactic gastrectomies for HDGC patients or a surgeon who has not done a TG for preventative reasons before. Ask the surgeon what their experience is. How many total gastrectomies have they performed? How many per year? Have any been prophylactic? Have any been for patients with the CDH1 mutation? What have their patient outcomes been? Have there been any complications? This may begin to feel like a job interview, and in a way, it is.
We have heard it suggested that an experienced surgeon likely performs 20-25 TGs annually. We decided to look for an expert to find out how to define “experienced.” Dr. Sam S. Yoon estimates that less than 1-2 dozen surgeons in the entire US perform that many TGs per year, and feels that 12 gastrectomies (1 per month) of any type (total, subtotal, distal) would qualify a surgeon as being in the top 1% of general or oncologic surgeons in the country. A handful of surgeons that we are aware of are:
Badgwell, Brian – MD Anderson Cancer Center, Houston TX
Kelly, MD, Kaitlyn – UW Health, Carbone Cancer Center, Madison, WI
Davis, MD, Jeremy – Marlene and Stewart Greenebaum Comprehensive Cancer Center, Baltimore MD
Kendrick, Michael L. – Mayo Clinic, Rochester MN
Roggin, Kevin – Medical University of South Carolina at Charleston
Mansfield, Paul – MD Anderson Cancer Center, Houston TX
Mullen, John – Massachusetts General Hospital, Boston MA
Norton, Jeff – Stanford University, Palo Alto CA
Strong, Vivian – Memorial Sloan Kettering Cancer Center, New York NY
Woo, Yanghee – City of Hope, Duarte CA
Yoon, Sam – Columbia University Irving Medical Center, New York NY
Will medical residents or students be involved in the procedure? Some surgeons work with surgeons-in-training or medical students. Of course, the expert surgeon will be in charge at all times, but it may be relevant to you to know whether others will be involved in your case.
When you are ready to move on to discuss the procedure, it makes sense, of course, to start with the details of TG, so you know and understand exactly what is being done on the operating table. What exactly does the procedure entail? Where will the esophagus and small intestine be cut, and how will the anastomosis (re-connections) be made? It may help to ask the surgeon to draw a picture for you. There are a few different ways to re-attach the small intestines to the esophagus. Specifically, a small jejunal “pouch” (sort of a mini-stomach made out of a portion of the small intestine) has been constructed during some TGs. However, research is conflicting regarding the outcome of this procedure. How will you ensure the proximal margin (the length of healthy esophageal mucosa that is cut beyond the gastric mucosa) of the stomach has been completely removed? It is necessary to get rid of all the gastric mucosa – you don’t want a remnant sitting beside a wound site. The rigor of ensuring this margin is resected is more significant than for non-HDGC surgery. For additional information about the surgical procedure see Prophylactic Gastrectomy for HDGC by S.S. Yoon et al.
NOTE: Pay close attention to the section titled “Materials and Methods”, in particular, the following sentence: “Reconstruction was performed with a Roux-en-Y reconstruction with a 60 cm Roux limb to prevent bile reflux.” This is a critical detail that has a significant impact on the quality of life following surgery. Refer to the HDGC Clinical Guidelines for more details about the surgical procedure.
- Consider printing this article and the HDGC Clinical Guideline to bring along to your appointment.
- What is the pre-operative workup? What tests do I need to have done before the surgery? Most operations include a pre-op workup including blood tests, an EKG, and possibly a chest X-ray. Is a bowel preparation required the day before the procedure?
- Is the procedure performed laparoscopically or open? What are the pros and cons of each method? Open gastrectomies are what we traditionally think of when we think about surgery – a large midline incision and pulling the skin, subcutaneous tissue, and muscles apart to open the abdominal cavity for the procedure. Laparoscopic techniques are newer and involve making some small openings in the abdomen, through which cameras and instruments are inserted to perform the procedure. In the United States, more total gastrectomies have been performed using the open technique, especially in HDGC patients, as it is critical to be sure that all gastric mucosa is removed. The first reported laparoscopic TG for HDGC was published in 2007.
NOTE: The following statement appears in the HDGC guideline on this topic: “There are potential advantages of laparoscopic gastrectomy with reduced wound pain and faster overall return to full activities, but conclusive evidence for the superiority of this approach is still lacking. Any surgeon proposing to do a laparoscopic PTG must be able to reassure the patient that this is without additional risk compared with open surgery.” - Do you re-attach the intestines with sutures (stitches) or staples? There are different instruments always being introduced into surgical procedures, and each technique has risks and benefits. Some surgeons hand-stitch the anastomosis, while others may use newer devices that staple the connection. It’s important to ask which one your surgeon will use and why.
- Do you insert a feeding tube at the time of surgery? While some patients may be capable of supporting themselves nutritionally for a short time after total gastrectomy, some surgeons may choose to insert a temporary feeding tube into the intestine (through the abdominal wall) during the gastrectomy in case complications arise during recovery and eating can’t be resumed. If this happens, liquid food can be inserted into the intestine via the feeding tube to provide nutrition until a patient can eat. If your surgeon does use a feeding tube, ask about the risks and benefits of that additional step in the procedure, and how long the feeding tube will be in place before it is removed.
- What type of lymph node dissection do you perform? Although the specific types of lymph node dissection are beyond the scope of this discussion, you may be curious to learn how many lymph nodes are taken out and examined when the stomach is removed.
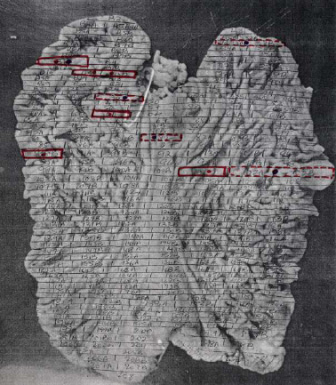
- How are the pathology specimens from my gastrectomy processed and inspected? As we have learned, HDGC is a type of cancer that originates through the stomach lining (mucosa) and can be very difficult to detect. It is imperative to know if your stomach contained cancer cells, and how many areas. Furthermore, if cancer is present, it is essential to see the depth of invasion (T-stage) since it is an indicator of the risk of recurrence and will determine whether chemotherapy should be given. Ask your surgeon if the pathologist who will be looking at the specimen has experience with or is knowledgeable about HDGC. To accurately determine the extent of cancer and its multifocality, it is necessary for the entire stomach to be microscopically examined and mapped. This process is only carried out by gastrointestinal pathologists in some academic centers and is not carried out in routine practice. To not adequately evaluate the entire stomach’s histopathology is to run the risk of not identifying a tumor focus that has invaded into the submucosa or beyond and therefore alters the therapeutic decision. This actual stomach map shows areas of gastric cancer in situ. Note: This information is the result of a consultation with Dr. Gregory Y. Lauwers and Dr. Parry Guilford.
- What can I expect in the post-operative period? Although we’d all like to get back on our feet as quickly as possible, it’s important to understand what your “new life” without a stomach will be like. What does the initial recovery process involve? How long am I expected to be in the hospital? When do you think I will be able to try eating for the first time after surgery? This is also an excellent time to ask any questions that you may have about the long-term complications of total gastrectomy.
Hopefully, you will feel more confident in making your decision after you have learned the answers to these questions.
*Please note, the above questions are not intended to provide medical advice to patients considering total prophylactic gastrectomy.