Hereditary Diffuse Gastric Cancer (HDGC) is one type of stomach cancer that is sometimes caused by a mutation in the CDH1 gene. These stomach cancer cells are diffuse, meaning that they are widely spread or scattered throughout the stomach, making it nearly impossible to detect them at an early stage. The recommended treatment to prevent the development of this aggressive form of stomach cancer in CDH1 gene mutation carriers is prophylactic (preventive) total gastrectomy – complete removal of the stomach. People with other types of stomach cancer may also undergo total gastrectomy as part of their treatment plan. Total gastrectomy is also performed to treat some non-cancer medical conditions. The reconstruction that follows total gastrectomy is referred to as Roux-en-y.
Preparing for Gastrectomy Choosing a Surgeon Living Without a Stomach Recovery
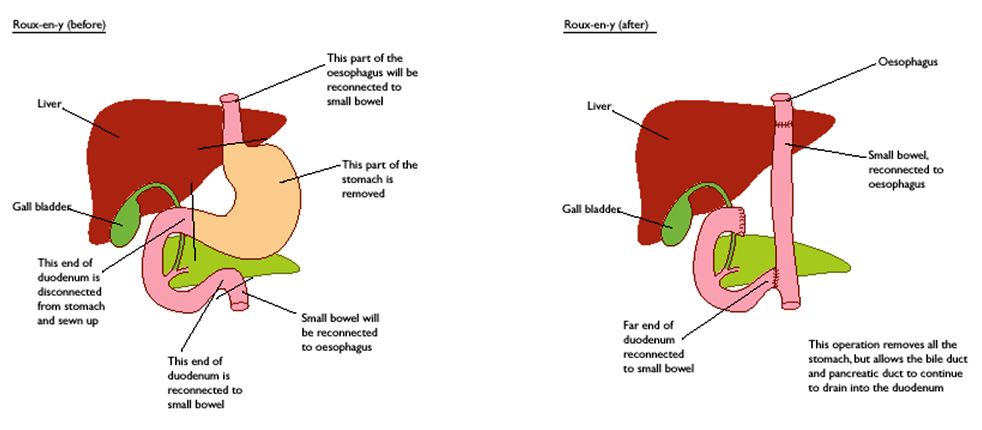
The Surgery
The diagrams below show the anatomy before and after reconstruction. The part of the small bowel that is initially cut at the lower end of the duodenum is extended straight up to meet the esophagus. The cut end of the duodenum is then reconnected to the small bowel. The entire procedure generally takes 4-5 hours followed by a hospital stay of 7-10 days. Often food and drink are withheld for the first 3-5 days, and moistened swabs are used to relieve dryness of the lips and mouth. The new construction needs time to heal and seal as leakage where the small bowel has been connected to the esophagus and the small intestine can be lethal. An x-ray test is often used to check for leaks before drinking and eating may resume. The first 2-4 weeks following surgery can be challenging. It may be uncomfortable or painful to eat, but this is a normal part of the healing process. Some surgeons will insert a feeding tube to supplement nutrition for a period of time following surgery – something to talk about prior to surgery. You may also find “About Your Gastrectomy Surgery” helpful.
Life After Surgery. Living without a Stomach.
The goal after surgery is to work toward settling into a “new normal”, allowing the body to heal and adjust to the loss of the stomach over time. At the same time, it is important to try to consume as many calories as possible to minimize rapid weight loss in the first few months following surgery, and to take in nutrients that the body needs to aid in the healing process. Starting to eat and drink again can be difficult, requiring a determined effort. It’s a lot of work, and sometimes feels as though life suddenly revolves around eating and drinking – what, when, where, and how much. Familiar sensations of hunger may be lost, replaced by feelings of weakness and emptiness. In the beginning eating and drinking is out of necessity, soon to become a habit, and eventually the desire to eat and enjoyment of food returns.
Most people will experience dumping syndrome at some point in time. Dumping syndrome is a group of symptoms that may occur 30-60 minutes after eating caused by rapid entry (or dumping) of food into the small intestine. Symptoms include nausea, vomiting, cramps, abdominal pain, diarrhea, and feeling full after eating only a small amount of food. Symptoms may also occur 90 minutes to 3 hours after eating caused by a rapid rise in blood sugar and then a rapid decrease in blood sugar. These symptoms are sweating, fast heart rate, and weakness, feeling tired or mental confusion. Nausea, heartburn, and gas are also common.
Symptoms can be controlled through eating habits and dietary changes. To avoid symptoms it is helpful to eat 6-8 small meals daily to avoid eating too much at one time. Drinking 1 hour before or after a meal rather than with a meal is recommended. Eating small amounts of food, taking small bites, and thoroughly chewing is important. Food tolerance varies by individual; learning is through trial and error, and it is important to remember that food tolerances continue to change over time. Foods high in sugar often lead to dumping syndrome, especially in the first three to six months.
Permanent weight loss of 20% of total body weight is typical within the first 3-6 months. Due to this rapid weight loss gallstones may develop, and can lead to the removal of the gallbladder. Osteoporosis becomes a concern, one of the many reasons to pay attention to nutrition and supplements following surgery. Maintaining proper vitamin levels is important. Vitamin supplements are important when nutrients cannot be acquired through diet alone. Monthly B12 shots are critical; it is not possible to absorb B12 without a stomach. Consuming enough calories to maintain activity levels is possible over time – people have returned to competitive running, hiking, and all sorts of things. Nutritious, high calorie, low sugar foods provide the best bang for the bite. Just finding those can be a challenge!
It may a year or two, but eventually, the body seems to adjust quite well to the absence of the stomach. Preventive Total Gastrectomy is curative for HDGC, the complete removal of the high risk and high anxiety of stomach cancer from your life. The best part about life after surgery . . . is life!
For more detailed information about caring for yourself following surgery refer to the Postsurgical Care and Nutrition section of the latest HDGC clinical guidelines.